
The Purpose of Poo
As you read this, your body is working hard to:
- Clear waste produced during its normal, healthy activities
- Remove compounds (e.g. hormones) from circulation that have completed their tasks
- Neutralise toxins that can harm your body, and
- Fight off pathogens (infectious organisms) that could otherwise make you sick
Once it’s completed these tasks, the next step is to eliminate these unwanted substances. It does this by packaging them up and sending them to your intestines to be eliminated in your poo!
So, How Often Should You Poo?
As your digestive tract is one of the main avenues for removing waste from your body, it’s ideal to pass at least one well-formed stool daily; this ensures the efficient clearance of toxins from your body. Anything less than this, and you might be experiencing constipation.
But why does this occur? What impact is it having within your gut? And most importantly, what can you do to address the underlying causes?
Read on to learn what to do when you don’t poo.

Constipation Characterised
The medical definition of chronic constipation (CC) involves experiencing the below symptoms for at least a three-month period:
- Hard or lumpy stools;
- Reduced frequency of defecation (less than three bowel motions per week);
- A sensation of not passing the entire stool (i.e. a feeling of incomplete evacuation); or
- Straining when passing a stool.
However, under this definition, straining to pass a hard stool each day, or only going several times a week, can be seen as ‘normal’, leading people to believe their symptoms are benign or harmless.
Unfortunately, this may not be the case. CC increases the risk of complications such as haemorrhoids, anal fissures, faecal impaction and faecal incontinence.
As your digestive tract is one of the main avenues for removing waste from your body, it’s ideal to pass at least one well-formed stool daily
Let’s Leave the Laxatives
For some, it may seem logical to simply take a laxative to move things along. Yes, laxatives can certainly help, however, whether they’re softening the stool or speeding up gut motility (the muscular contractions of your intestines that move the stool through the colon), they’re not addressing the underlying dysfunction that triggers constipation. Additionally, regular laxative use carries the risk of the bowel developing a dependence on them to pass a stool.
Addressing the true cause of constipation requires us to examine the health of the gut, with a special spotlight on the microbiome.
The Microbiome-Constipation Connection
Your intestinal microbiome is a living colony of 38 trillion beneficial bacteria, yeasts and fungi that work synergistically to keep your gut, immune system and entire body healthy. When it comes to bowel regularity, your microbiome plays two hugely important roles:
- Converts the fibre from your food into short-chain fatty acids (SCFAs). SCFAs regulate your gut motility as well as provide fuel for your gut cells, keeping your digestive system healthy. Insufficient fibre intake, or not having enough good gut bacteria, can cause low levels of SCFAs, decreasing gut motility and leading to constipation. In fact, research has shown that constipated patients have lower levels of SCFAs compared to those with diarrhoea.
- Prevents pathogenic (bad) organisms from overgrowing in the gut. These unwanted organisms can trigger microbiome-disrupting inflammation, and also produce gasses such as methane, which slow gut motility. Together, these negative effects can produce constipation.
In order to remedy your microbiome issues and eliminate your constipation, there are two key ingredients you can call on.
Prebiotics Promote the Poo
The first ingredient to look for when restoring the microbiome to treat constipation is partially hydrolysed guar gum (PHGG). PHGG is prebiotic, which is a group of fibres that provide your beneficial bacteria with the food to make SCFAs. Research shows 5 g/d of PHGG to provide particular benefit to those with constipation, demonstrating the capacity to soften the stool, increase the weekly number of bowel motions, and decrease abdominal pain, straining with bowel motions, and laxative use.
Research shows 5 g/d of PHGG to provide particular benefit to those with constipation, demonstrating the capacity to soften the stool, increase the weekly number of bowel motions, and decrease abdominal pain, straining with bowel motions, and laxative use.
The Strain that Stops the Strain
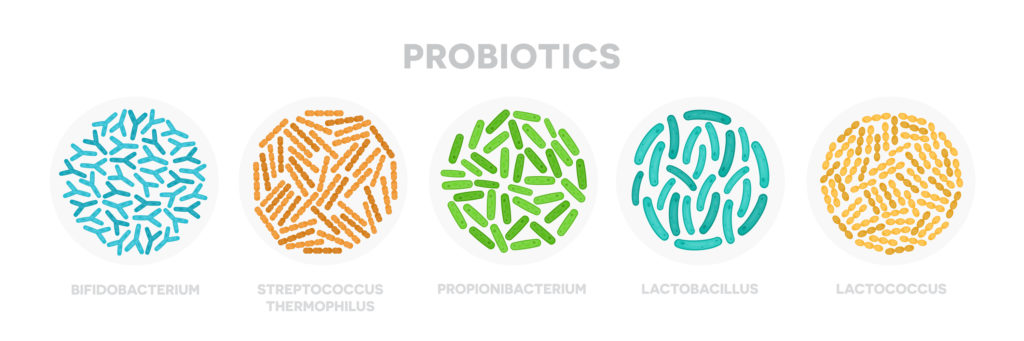
The second ingredient is the probiotic strain Lactobacillus plantarum 299v. Probiotics are live, beneficial microbes that support the health of your gut and intestinal microbiome. To read more on what probiotics are and why selecting the right strain is important, here.
A primary action of probiotics, including 299v, is to help the beneficial organisms within your microbiome to grow and flourish. This creates more good bacteria that then produce more SCFAs, which we now know is very useful for combatting constipation! Beyond this, 299v can also produce antimicrobial substances that prevent pathogenic microbes from surviving within the gut, reduce inflammation within your digestive tract, and prevent pathogenic organisms from attaching to your gut lining.
Together, these actions result in increased stool softness, gut motility, and the feeling of complete evacuation, whilst also reducing symptoms such as abdominal pain.
Get Things Moving
If you’re moving your bowels less than once a day, passing hard stools, straining, or experiencing a sense of incomplete evacuation, your microbiome may need support. Taking PHGG and 299v to ensure good gut motility and promote SCFA production may be just what you need to get things moving. Book in for a consult about accessing this constipation-combatting duo today!
Reference
Black CJ, Ford AC. Chronic idiopathic constipation in adults: epidemiology, pathophysiology, diagnosis and clinical management. Med J Aust. 2018 Jul 16;209(2):86-91. PMID: 29996755.
Ducrotté P, Sawant P, Jayanthi V. Clinical trial: Lactobacillus plantarum 299v (DSM 9843) improves symptoms of irritable bowel syndrome. World J Gastroenterol. 2012 Aug 14;18(30):4012-8. doi: 10.3748/wjg.v18.i30.4012.
Johansson ML, Nobaek S, Berggren A, Nyman M, Björck I, Ahrné S, et al. Survival of Lactobacillus plantarum DSM 9843 (299v), and effect on the short-chain fatty acid content of faeces after ingestion of a rose-hip drink with fermented oats. Int J Food Microbiol. 1998 June 30;42(1-2):29-38. PMID: 9706795.
Karlsson C, Ahrné S, Molin G, Berggren A, Palmquist I, Fredrikson GN, et al. Probiotic therapy to men with incipient arteriosclerosis initiates increased bacterial diversity in colon: a randomised controlled trial. Atherosclerosis. 2010 Jan;208(1):228-33. PMID: 19608185.
Kujawa-Szewieczek A, Adamczak M, Kwiecień K, Dudzicz S, Gazda M, Więcek A. The effect of Lactobacillus plantarum 299v on the incidence of Clostridium difficile infection in high risk patients treated with antibiotics. Nutrients. 2015;7(12):10179-88. doi:10.3390/nu7125526.
Polymeros D, Beintaris I, Gaglia A, Karamanolis G, Papanikolaou IS, Dimitriadis G, et al. Partially hydrolysed guar gum accelerates colonic transit time and improves symptoms in adults with chronic constipation. Dig Dis Sci. 2014 Sep;59(9):2207-14. doi: 10.1007/s10620-014-3135-1.
Ringel-Kulka T, Choi CH, Temas D, Kim A, Maier DM, Scott K, et al. Altered colonic bacterial fermentation as a potential pathophysiological factor in irritable bowel syndrome. Am J Gastroenterol. 2015;110(9):1339-46. doi: 10.1038/ajg.2015.220.
Seddik HA, Bendali F, Gancel F, Fliss I, Spano G, Drider D. Lactobacillus plantarum and its probiotic and food potentialities. Probiotics Antimicrob Proteins. 2017 Jun;9(2):111-122. doi: 10.1007/s12602-017-9264-z.